In this section, you'll find everything you need to know about our anaesthesia and pain medicine training programs; how to get your overseas qualifications certified by the college so you can practice in Australia or New Zealand; how you can join our continuing professional development (CPD) program (even if you’re not a member of the college); and the range of lifelong courses and resources available to support our fellows and trainees throughout their career.

Information on the ANZCA, RGA, and DHM training programs and the joint ANZCA-CICM training pathway

Information on the Faculty of Pain Medicine Training Program and Procedures Endorsement Program.
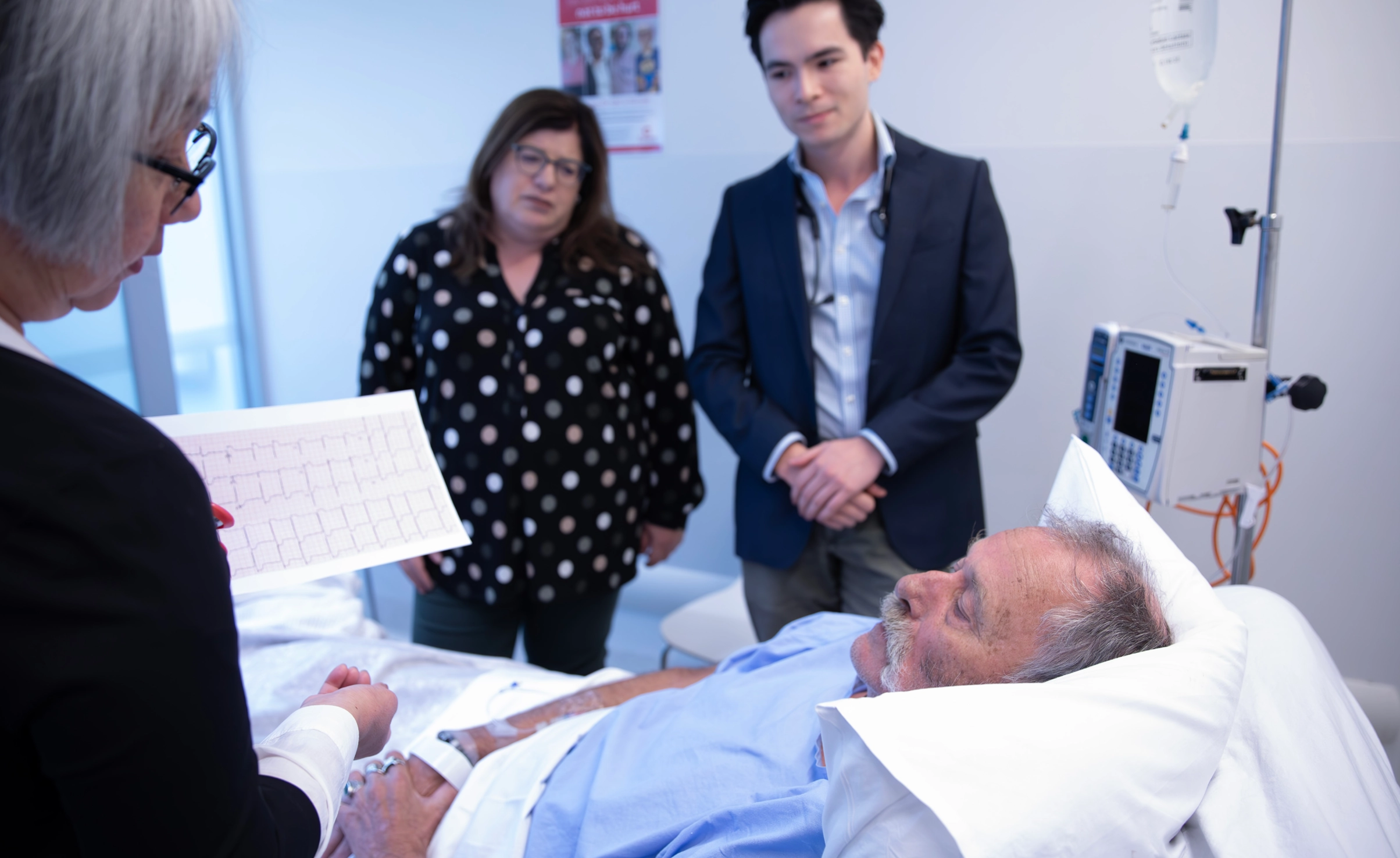
The ANZCA Course in Perioperative Medicine enables specialist doctors enhance their skills and knowledge in perioperative medicine.

If you trained as a specialist anaesthetist or specialist pain medicine physician overseas, we offer several SIMG pathways to practice in Australia or New Zealand.

Effective Management of Anaesthetic Crises (EMAC) is a simulation-based course focused on managing anaesthetic emergencies, and is a compulsory requirement of the anaesthesia training program.

Elevate how you educate with the ANZCA Educators Program (AEP).

Every year, ANZCA offers a number of bursaries to assist trainees who are experiencing financial hardship. Eligible anaesthetic and pain medicine trainees can receive up to a 50 per cent reduction in their annual training fees. All applicants will also receive an extension to the annual training fee due date.

ANZCA and FPM are accredited by the Australian Medical Council (AMC) and Medical Council of New Zealand (MCNZ) to deliver our training programs, SIMG assessment process and continuing professional development program.
Revised Reconsideration, Review, and Appeal Policy and the Special Consideration Policy.

Participating in a continuing professional development (CPD) program is compulsory for specialist registration in Australia and New Zealand.
Information, resources and support related to ANZCA & FPM's education programs, including the primary exam (PEx) reading list.



.webp?language=en)