The CLIP-II trial, an NHMRC funded phase III multicentre blinded randomised controlled clinical non-inferiority trial of cryopreserved platelets vs. conventional liquid-stored platelets for the management of post-surgical bleeding, commenced recruitment in August 2021. Eleven sites participated in the trial: the Royal Prince Alfred Hospital, Prince Charles Hospital, Townsville University Hospital, the Austin Hospital, Gold Coast University Hospital, St. Vincent’s Hospital Melbourne, Westmead Hospital, the Alfred Hospital, Liverpool, the Victorian Heart Hospital and the Royal Melbourne Hospital. Study recruitment was reached on the 15 April 2024 with 388 participants randomised with 202 participants receiving ‘study platelets’.
In New Zealand, an investigative team led by Dr Shay McGuinness and Associate Professor Rachael Parke, has received funding from the NZ Health Research Council (HRC) to run a parallel protocol using cryopreserved platelets manufactured by a slightly different technique.
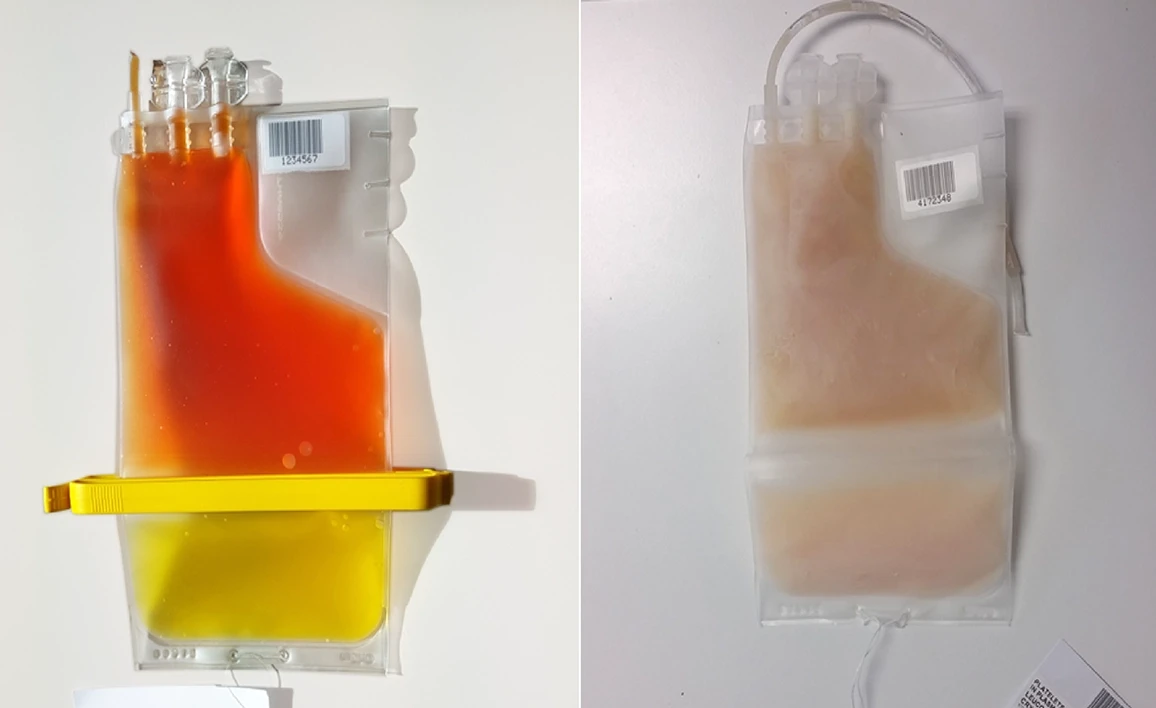
Platelets are stored at 22°C to prolong circulating time after transfusion. This risks bacterial growth, limiting shelf-life to five days. Freezing, using dimethylsuphoxide (DMSO) as a cryoprotectant, extends shelf-life to two years. However, despite development by the US Navy in the 1970s, only one clinical trial, in which only 24 patients received cryopreserved platelets, has been published. This small study found cryopreserved platelets were safe and more effective than liquid-stored platelets. Funded by an ANZCA Academic Enhancement Grant, the CLIP investigators (a collaboration of the Australian Defence Force, the Australian Red Cross Blood Service led by Dr Denese Marks, and civilian hospital clinicians around Australia) have completed the CLIP-I pilot trial, demonstrating the feasibility and safety of a protocol comparing frozen and liquid platelets in cardiac surgery patients. The CLIP investigators secured a $A1.85 million NHMRC grant to run a definitive trial in 10 to 12 Australian hospitals. If cryopreserved platelets are as safe and effective as hypothesised, the study will change the way platelets are stored worldwide, and make platelet transfusions possible in the many small hospitals that currently have no platelet blood bank. Study design: Randomised, double-blind non-inferiority phase III clinical trial in high-risk adult cardiac surgery patients.
Study size
808 patients randomised to achieve 202 patients transfused platelets (101 in each group). Primary outcome: Volume of post-surgical bleeding in the first 24 hours from the time of ICU admission.
Secondary outcomes
Transfusion and fluid resuscitation requirement; Bleeding Academic Research Consortium composite bleeding outcome; adverse effects (specifically: DMSO toxicity; infection; venous thromboembolism; arterial occlusion; need for surgical intervention; and acute respiratory distress syndrome); total estimated healthcare cost.
Study duration
Four years.
The Australian National Health and Medical Research Council A$1.8 million
Health Research Council of New Zealand NZ$1,399,921.00.
Australian Red Cross Lifeblood is providing in-kind support in the form of funding some of the investigational product (the platelets).
The CLIP-II study is endorsed by the Australian and New Zealand Intensive Care Society Clinical Trials Group (ANZICS-CTG), the ANZCA Clinical Trials Network, and the Australian and New Zealand Society of Cardiac and Thoracic Surgeons.
ClinicalTrials.gov Identifier: NCT03991481
| Australian Hospitals |
| Alfred Hospital |
| Austin Health |
| Gold Coast University Hospital |
| Liverpool Hospital |
| Royal Prince Alfred |
| Royal Melbourne Hospital |
| St Vincents Hospital, Melbourne |
| The Prince Charles Hospital |
| Townsville University Hospital |
| Westmead Hospital |
| Victorian Heart Hospital |
| New Zealand Hospitals |
| Auckland City Hospital CVICU |
| Christchurch Hospital |
| Dunedin Hospital |
| Waikato Hospital |
| Wellington Hospital |
For further information about this study, please contact the ANZIC-RC CLIP-II Project Manager, Belinda Howe by email.
Reade MC, Marks DC, Howe B, McGuinness S, Parke R, Navarra L, Charlewood R, Johnson L, McQuilten Z; CLIP-II and CLIPNZ-II Investigators.; CLIP-II and CLIPNZ-II Investigators. Cryopreserved platelets compared with liquid-stored platelets for the treatment of surgical bleeding: protocol for two multicentre randomised controlled blinded non-inferiority trials (the CLIP-II and CLIPNZ-II trials). BMJ Open. 2022 Dec 20;12(12):e068933. doi: 10.1136/bmjopen-2022-068933. PMID: 36600425; PMCID: PMC9772641.
Flint AWJ, Bailey M, Reid CM, Smith JA, Tran L, Wood EM, McQuilten ZK, Reade MC. Preoperative identification of cardiac surgery patients at risk of receiving a platelet transfusion: The Australian Cardiac Surgery Platelet Transfusion (ACSePT) risk prediction tool. Transfusion. 2020 Oct;60(10):2272-2283. doi: 10.1111/trf.15990. Epub 2020 Aug 5. PMID: 32757209.
Reade MC, Marks DC, Bellomo R, Deans R, Faulke DJ, Fraser JF, Gattas DJ, Holley AD, Irving DO, Johnson L, Pearse BL, Royse AG, Wong J; Cryopreserved vs Liquid Platelet (CLIP) Investigators, the Australian and New Zealand College of Anaesthetists Clinical Trials Network, and the Australian and New Zealand Intensive Care Society Clinical Trials Group. A randomized, controlled pilot clinical trial of cryopreserved platelets for perioperative surgical bleeding: the CLIP-I trial (Editorial, p. 2759). Transfusion. 2019 Sep;59(9):2794-2804. doi: 10.1111/trf.15423. Epub 2019 Jul 10. PMID: 31290573.
Reade MC, Marks DC, Johnson L, Irving DO, Holley AD. Frozen platelets for rural Australia: the CLIP trial. Anaesth Intensive Care. 2013 Nov;41(6):804-5. PMID: 24180724.
Dumont LJ, Slichter SJ, Reade MC.Cryopreserved platelets: frozen in a logjam?Transfusion. 2014 Aug;54(8):1907-10. doi: 10.1111/trf.12758. PMID: 25130330.
Johnson L, Reade MC, Hyland RA, Tan S, Marks DC. In vitro comparison of cryopreserved and liquid platelets: potential clinical implications. Transfusion. 2015 Apr;55(4):838-47. doi: 10.1111/trf.12915. Epub 2014 Nov 5. PMID: 25371169.
Marks DC, Johnson L, Reade MC. A clinical trial of frozen platelets: rationale, protocol and pilot analysis plan. Vox Sang. First published: 22 January 2018.
McGuinness S, Charlewood R, Gilder E, Parke R, Hayes K, Morley S, Al-Ibousi A, Deans R, Howe B, Johnson L, Marks DC, Reade MC; Australian and New Zealand College of Anaesthetists Clinical Trials Network; Australian and New Zealand Intensive Care Society Clinical Trials Group. A pilot randomized clinical trial of cryopreserved versus liquid-stored platelet transfusion for bleeding in cardiac surgery: The cryopreserved versus liquid platelet-New Zealand pilot trial. Vox Sang. 2022 Mar;117(3):337-345. doi: 10.1111/vox.13203. Epub 2021 Sep 28. PMID: 34581452.