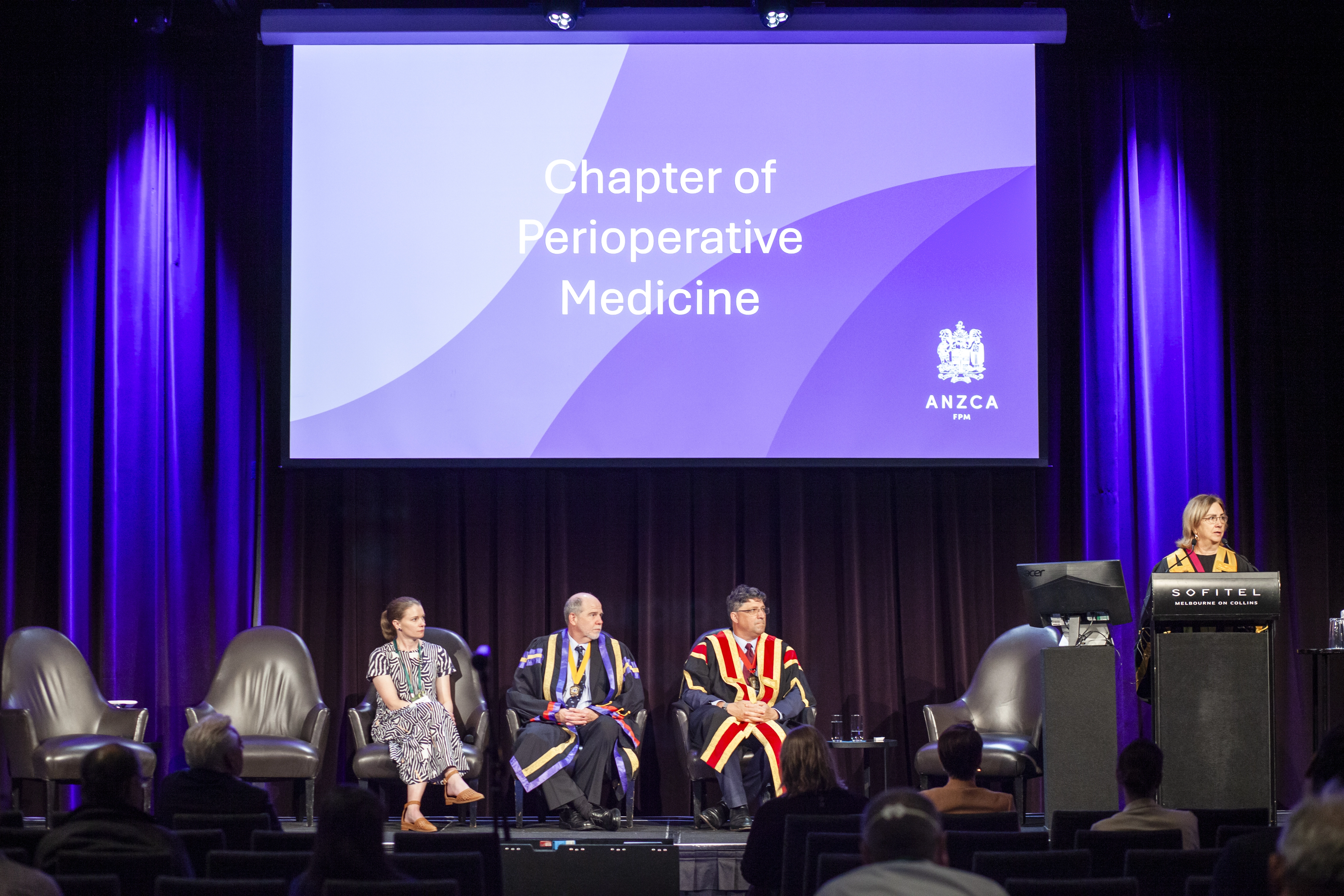
Launched in 2023, the ANZCA Course in Perioperative Medicine is a key element of ANZCA’s strategic plan to establish an integrated, patient-centred approach to perioperative care in Australia and New Zealand.
The course is the first in the world to offer clinical immersion with guidance and support from graduates of the Chapter of Perioperative Medicine. It is overseen by the Board of the Chapter of Perioperative Medicine and the Chapter of Perioperative Medicine Education and Assessment Committee.
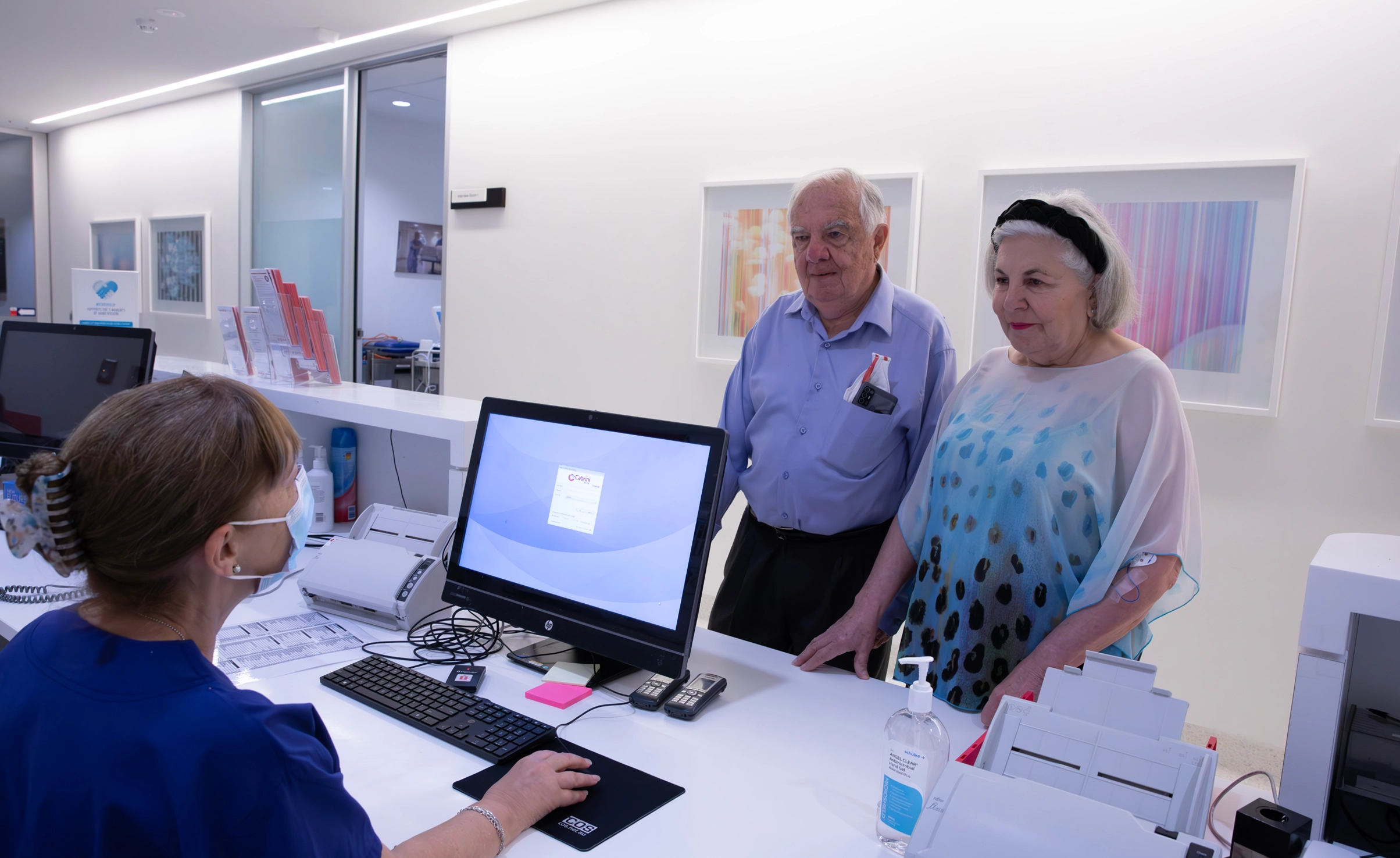
This certification enables specialist doctors, such as anaesthetists, surgeons, physicians, intensivists, and general practitioners to enhance their skills and knowledge in perioperative medicine.
Information on the course structure, modes of delivery, eligibility, and enrolment.

Fees, dates, and resources related to the ANZCA Course in Perioperative Medicine.

An engaging clinical experience is essential in shaping competent perioperative medicine practitioners.

ANZCA Course in Perioperative Medicine has several roles that are crucial to the success of course delivery. All roles available are open to the graduates of the Chapter of Perioperative Medicine (ANZCA).

Learn about recent changes to the ANZCA Course in Perioperative Medicine — including updates to the workshop component, the reasons for these changes, the new structure, and updated requirements.
From literature reviews to advocacy, find out what we're doing to make the case for reform and resource allocation by governments, funders, and administrators.

The Perioperative Care Framework was developed by the Perioperative Care Working Group approved by ANZCA Council in December 2021, and updated in December 2023.

The Chapter of Perioperative Medicine Board reports to the ANZCA Council on developing and implementing an integrated perioperative care model and educational offerings for Australia and New Zealand, focusing on professional practice, clinical quality, and patient safety.