The Australian and New Zealand College of Anaesthetists (ANZCA) welcomes the announcement of a new $3.7 million Medical Research Future Fund (MRFF) grant for a world-first study set to reshape monitoring practices for patients undergoing open-heart surgery.
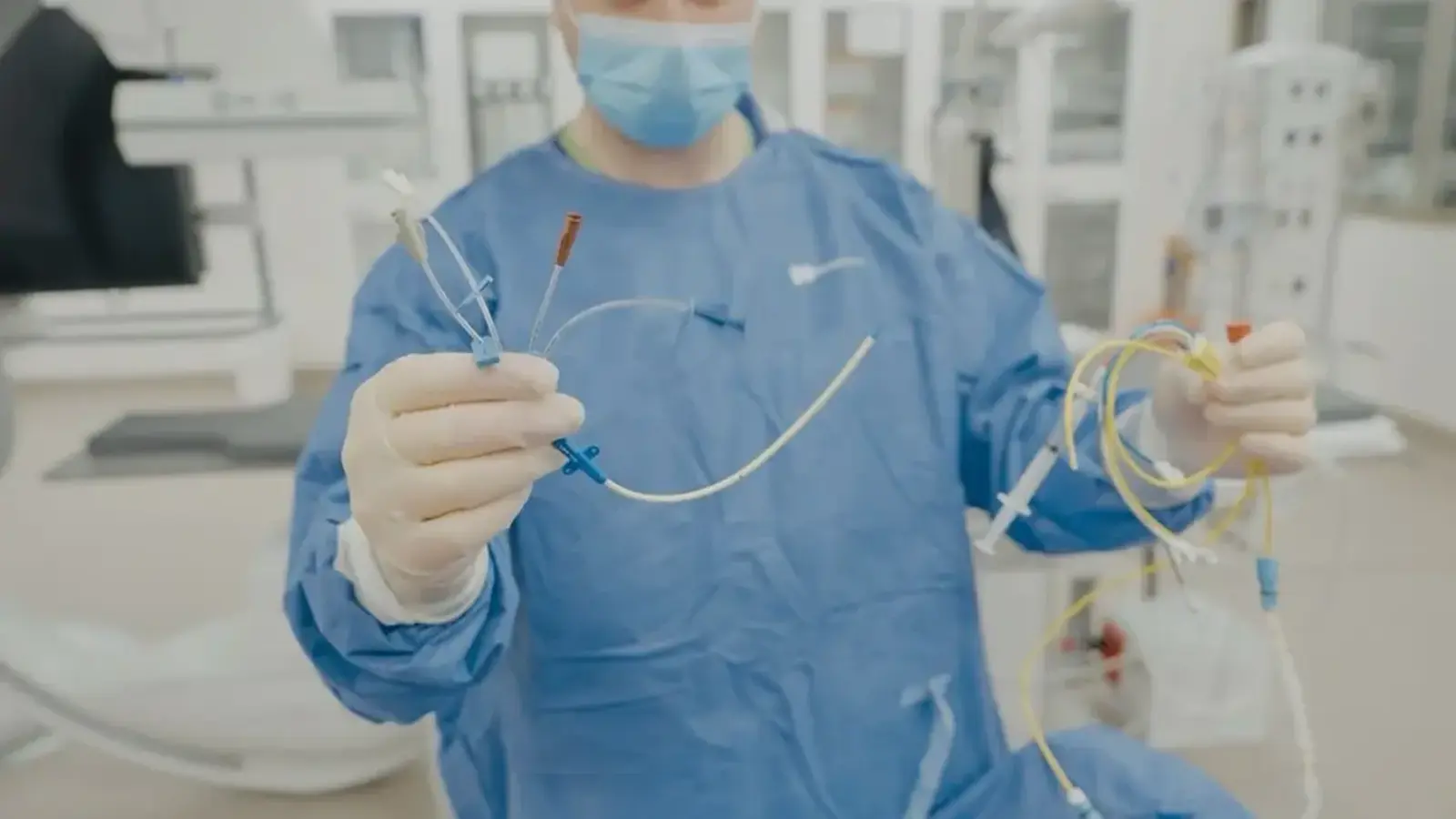
Led by Dr Luke Perry, anaesthesia registrar at the Victorian Heart Institute, the pulmonary artery catheters in low-risk cardiac surgery (PUMA) trial will compare the long-standing use of pulmonary artery catheters (PACs) with a simpler, less invasive central venous catheter (CVC).
The 2000-patient trial will begin recruitment in Australia at hospitals across the ANZCA Clinical Trials Network (CTN) that perform cardiac surgery, and internationally in 2026.
“Cardiac anaesthesia has relied on pulmonary artery catheters for decades, yet high-quality evidence for their benefit in modern cardiac surgery is still lacking,” Dr Perry says.
“PUMA aims to provide the clarity clinicians and patients have been waiting for.”
PACs can provide detailed information about blood flow and pressure during cardiac surgery but may expose patients to complications and unnecessary interventions.
Trial co-investigator Associate Professor Lachlan Miles, Head of Research, Department of Anaesthesia, at Austin Health, said the trial will answer a critical question for anaesthetists: “Does this level of invasiveness actually improve outcomes, or is it low-value care?”
Designed in partnership with cardiac surgery patients and their families, PUMA focuses on outcomes they say matter most: survival, fewer complications, and getting home sooner.
If CVCs are shown to be no worse than a PAC, the findings could reduce procedural risk, shorten ICU stays, lower healthcare costs, and cut the environmental footprint of cardiac surgery.
PUMA is supported by major national and international collaborators including Weill Cornell Medicine, Monash Health, the University of Melbourne, and peak cardiac advocacy groups.
Banner image: PUMA Lead Dr Perry demonstrating the pulmonary artery catheter (right) with the less invasive central venous catheter (left)



